New research reveals how COVID-19 triggers cytokine storms
Scientists at the Dunn School have shown that SARS-CoV-2, the virus that causes COVID-19, can alter macrophages and potentially trigger hyper-inflammation (a ‘cytokine storm’) in patients. This research unravels a possible mechanism that can be targeted for future treatments to alleviate the severity of symptoms and save lives.
Published in the journal Nature Immunology, the research is a part of international efforts made by leaders in infectious diseases from the University of Oxford, University of Hong Kong, and Ghent University, supported by a UKRI COVID19 grant. Dr Deeksha Munnur, who led the study, said “During the current pandemic, the scientific community has come together to pool resources and expertise towards a common goal. Whilst this was a collaborative effort between different institutes, having access to the BSL2 and 3 facilities at the Dunn School will make the type of research we are interested in more achievable in future.”
A link between SARS-CoV-2 and ISGylation in macrophages
ISG15 is a small ubiquitin-like protein that can be added onto different proteins to modify their activity, and is used in host defense mechanisms during infection. This process is often subverted by viruses to disrupt host immune responses. “We showed that infection by Zika and influenza promotes cellular ISGylation and were curious if the same principle applies to SARS-CoV-2,” the principal investigator of this study, Dr Sumana Sanyal, said. By investigating if SARS-CoV-2 functions similarly as other viruses in host macrophages, the authors discovered that global ISGylation of proteins in macrophages dwindled during SARS-CoV-2 infection even in the presence of type I interferon, in contrast to Zika and influenza viruses. This is not caused by a lowered ISGylation activity, because SARS-CoV-2 increased the expression of enzymes that catalyse ISGylation. Therefore, the phenomenon is likely caused by deISGylation, the process of removal of ISGylation from proteins. The authors show that the papain-like protease (PLpro), a protein encoded by SARS-CoV-2, is able to trigger cellular de-ISGylation in infected cells, or upon expression of PLpro alone in uninfected cells. They also found that this phenomenon resulted in increased secretion of free ISG15 from these macrophages.
Compromised ISGylation in macrophages results in an immune system overreaction
By monitoring how SARS-CoV-2-infected macrophages behave, the authors observed that macrophages became malfunctional with reduced antigen presentation and elevated secretion of pro-inflammatory cytokines. Mechanistically, the authors propose that PLpro from SARS-CoV-2 induces deISGylation, which changes the metabolic balance of macrophages. This then unleashes the host’s inflammatory response, which is normally suppressed through ISGylation. Secretion of the surplus intracellular ISG15 by macrophages further exacerbates the overreaction of the immune response. “Our work helps to delineate the effect of altered free versus conjugated ISG15 in macrophages, and show that SARS-CoV-2 can disrupt immune response in macrophages, potentially driving the onset of lymphopenia, a state of reduced white blood cells level, and increased inflammation, both hallmarks of severe COVID-19,” Dr Sanyal added. Taken together, these findings suggest a pivotal mechanism explaining the origin of the cytokine storm observed in COVID-19 patients.
A road to save lives
A hyperactive immune response characterized by an overwhelming release of pro-inflammatory cytokines is often associated with high mortality and occupancy of intensive care unit (ICU) by COVID-19 patients. While studying the mechanism of COVID-19-caused cytokine storm contributes to global efforts in understanding this devastating disease, it can also help identify important proteins on this pathway that can be targeted for therapeutic interventions. “I feel very fortunate to have had this opportunity to use my research skills to help understand the immunology of this virus. Our work could help further advance the therapeutic side of the fight against SARS-CoV-2 by using PLpro as a druggable candidate,” Dr Munnur enthusiastically said. Further development may save lives and alleviate the burden of COVID-19 on our medical system.
Written by Isaac Siu-Shing Wong (Raff Lab) @ISiuShingWong. Edited by Alexandra Bisia (Robertson Lab) @AlexandraBisia.
Research article: Deeksha Munnur, Qiwen Teo, Denzel Eggermont, Horace H. Y. Lee, Fabien Thery, Julian Ho, Sophie Wilhelmina van Leur, Wilson W. S. Ng, Lewis Y. L. Siu, Antje Beling, Hidde Ploegh, Adan Pinto-Fernandez, Andreas Damianou, Benedikt Kessler, Francis Impens, Chris Ka Pun Mok and Sumana Sanyal (2021). Altered ISGylation drives aberrant macrophage-dependent immune responses during SARS-CoV-2 infection. Nature Immunology. 22, 1416–1427.
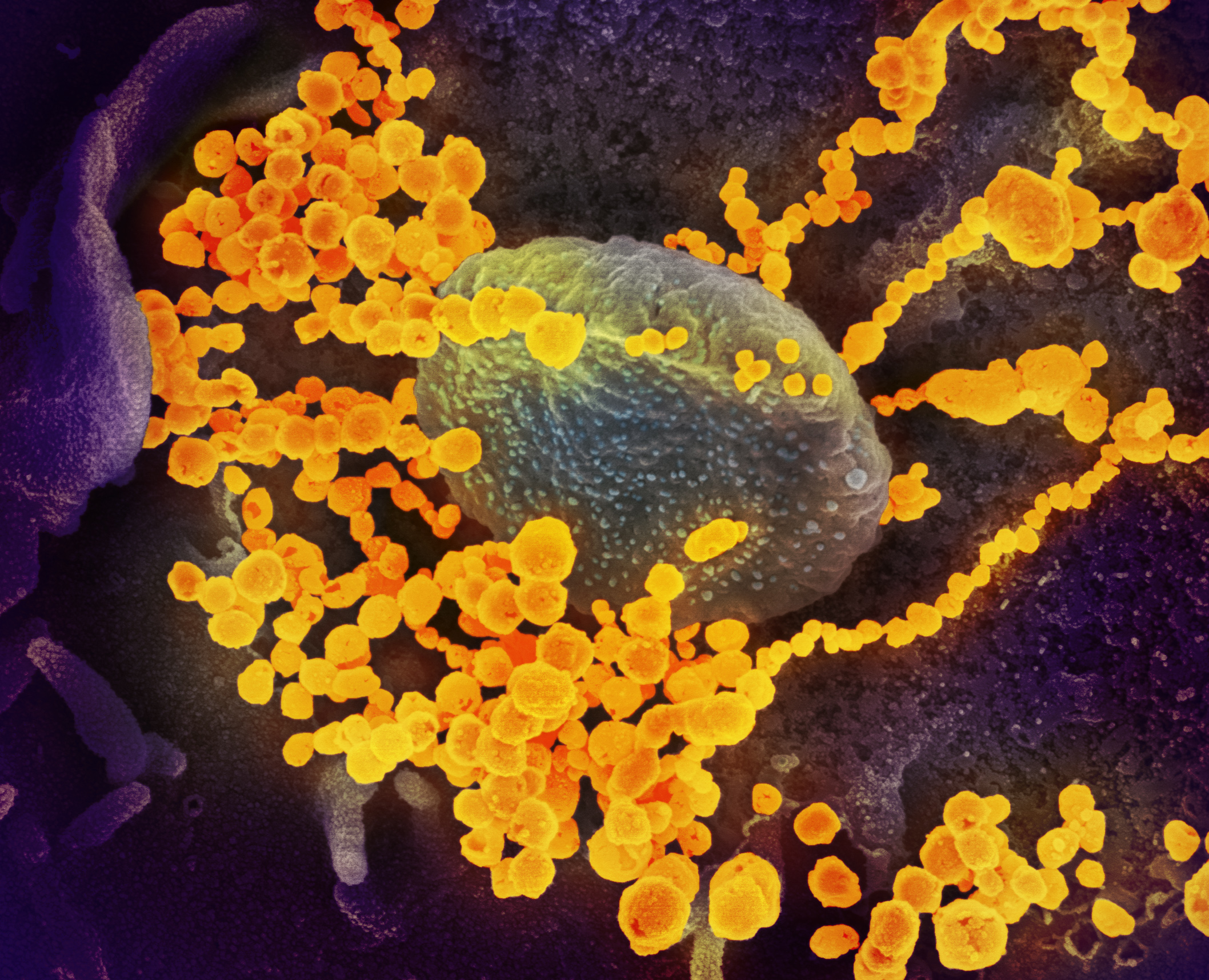
*Image credit: NIH NIAID